January 19, 2026
Detecting (often hidden) heart failure in general practice with NLP
Ruben Styl & Evi Noppe

Detecting (often hidden) heart failure in general practice with NLP

The problem: heart failure is often hidden in the EMR
Heart failure is one of the major challenges in healthcare. Paradoxically, it is partly a result of our own success: because we treat heart attacks, valvular disease, and hypertension increasingly better, patients live longer, but often with a damaged heart that eventually fails.
In Belgium, an estimated 250,000 people live with heart failure. In those over 70, the prevalence rises to almost 1 in 4. Due to aging and the increase in obesity, this number continues to rise. This has a major impact: reduced quality of life and frequent hospitalizations with high healthcare costs.
Why is heart failure so difficult to recognize?
The symptoms of heart failure—shortness of breath, fatigue, swollen ankles—can fit multiple conditions. In older patients, we often attribute them to age, overweight, or reduced fitness. And although echocardiography is well accessible in Belgium, biomarkers such as NT-proBNP are not systematically requested, partly because they are not yet reimbursed in general practice.
HFpEF: the invisible variant
Particularly challenging is heart failure with preserved ejection fraction (HFpEF). In this form, the heart still pumps well, but no longer fills smoothly. As a result, standard resting tests are often completely normal. This form is most common in the older population.
A registration problem
Research in general practice shows that the registration of heart failure is far from optimal:
- Over-registration: In the Belgian OSCAR-HF study, up to 47% of patients with a heart failure code in the EMR had no heart failure upon further evaluation.1 Often these are working diagnoses or excluded differential diagnoses that were never corrected.
- Under-registration: The same study showed that an extensive audit led to 74% more identified heart failure patients. More than two-thirds of them previously had no heart failure diagnosis in their file.
- Communication gap with the specialist: Notably, the heart failure diagnosis is often not explicitly mentioned in cardiologist reports. The diagnosis was missing in 24% of HFrEF cases, 49% of HFmrEF cases, and as much as 66% of HFpEF cases.
As a result, a significant portion of heart failure patients do not receive the follow-up and treatment they need. A simple identification method is therefore necessary.
The traditional approach: effective but time-consuming
There are methods to systematically detect heart failure. The OSCAR method, developed in Belgium, combines an extensive audit with manual file review.1
An audit searches the EMR for heart failure diagnoses, risk factors, and typical medications. The general practitioner then reviews the list of possible patients. Then comes the time-consuming step: for each possible heart failure patient, someone must go through the entire file—lab results, cardiology letters, echo reports—to objectify whether there is actually heart failure.
This method works, but requires a significant time investment per patient, which is why it is usually not performed in practice. Regularly repeating the audit for quality improvement is almost impossible.
Moreover, the traditional flowchart misses an important portion of HFpEF patients, in whom the “hard” objective criteria are often lacking.
How Co-VIHP makes a difference
What does Co-VIHP do exactly?
The platform automatically reads all unstructured text in the EMR: consultation notes, specialist letters, discharge reports, echo reports. The NLP algorithm (natural language processing) recognizes clinical concepts: symptoms, diagnoses, medications, laboratory values, echocardiographic parameters, and codes them into structured codes (SNOMED CT and LOINC). This makes information from free text searchable and usable for diagnostic algorithms.
Why is this groundbreaking?
- Easily get an overview of the practice’s heart failure population: The model allows automatic identification of the heart failure patient population in general practice. What manually requires a significant time investment now happens in minutes for an entire practice population. For general practitioners and VIHPs, this means that managing this population becomes feasible.
- Works on an uncoded file: In general practice, mainly major diagnoses are coded. Echocardiographic parameters and other cardiological findings are unstructured in letters. Co-VIHP extracts this information directly from the text. A cardiologist letter mentioning “severe diastolic dysfunction” is recognized and structured.
- Traceable: Each extracted parameter links back to the source document so it can be verified.
The research
In an ongoing master’s thesis, Ruben Styl and Evi Noppe—both general practitioners in training—are testing the Co-Medic platform in two Flemish general practices.
The research questions:
Can NLP execute a diagnostic algorithm to objectify heart failure? This compares a manual file review with one performed by Co-VIHP.
Does NLP detect hidden HFpEF? The researchers developed an additional case-finding method based on the H2FpEF score, which identifies patients with high HFpEF probability.
How accurate is NLP compared to the manual method? And how much time does it save concretely?
Co-VIHP in practice: mapping your chronic population
This thesis is part of the Co-VIHP vision: proactively mapping chronic patient populations in general practice so that care can be easily coordinated.
From reactive to proactive
Traditionally, the general practitioner waits until patients present with complaints. In recent years, there has been an evolution toward early detection of patients with health risks and continuous quality improvement. The insufficient availability of structured data in general practice remains a major barrier to such population-level care today.
With Co-VIHP, we want to remove this data barrier and help general practices identify and monitor conditions such as heart failure, osteoporosis, COPD, diabetes, and chronic kidney disease.
Curious about the results?
The thesis is currently running in two Flemish practices. Once the results are known, we will share them here.
Want to learn more about how Co-VIHP can support your practice in population management?
Schedule a conversationThis research is conducted by Ruben Styl and Evi Noppe under the supervision of prof. dr. Miek Smeets and co-supervision of prof. dr. Andreas Gevaert.
References
1 Smeets M, Vaes B, Aertgeerts B, et al. Impact of an extended audit on identifying heart failure patients in general practice: baseline results of the OSCAR-HF pilot study. ESC Heart Fail. 2020;7(6):3950-3961.Want to explore Co-Medic further?
Connect with our team or keep reading more insights from our blog archive.
Related articles
Jan 15, 2026
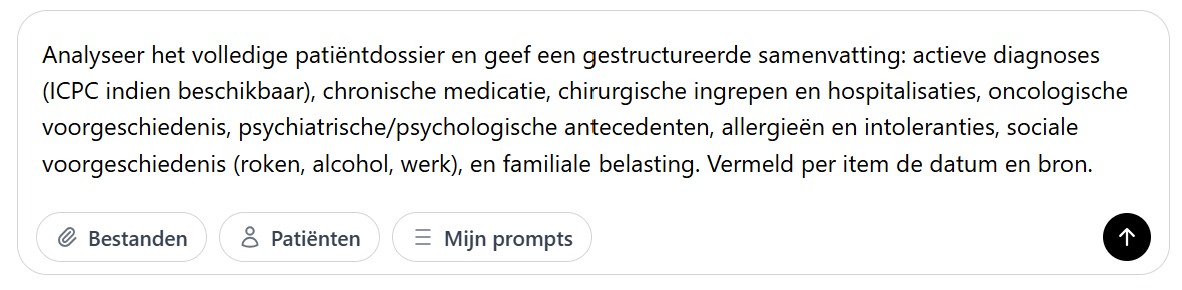
Practice case: 4 hours time savings with Co‑Chat
How Co-Chat saves a general practitioner four hours of work per dossier by bringing scattered dossier data together in one clear overview.
Read more
Jan 6, 2026
Efficient letter processing in a group practice: where do you start?
Dr. Bram Spinnewijn shares how his group practice organizes daily correspondence using the Co-Medic letter processor.
Read more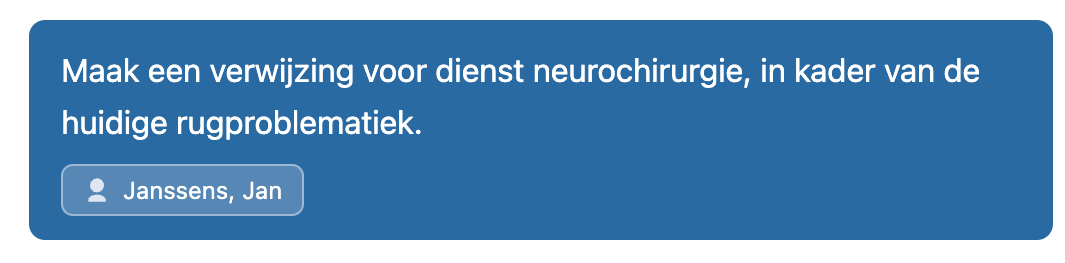
Dec 10, 2025
Webinar: AI in general practice
Together with ASGB Kartel we hosted a webinar about AI use cases for primary care.
Read more