October 10, 2022
Telemonitoring convention for COVID-19
Ruben Styl

1. INTRODUCTION
The pressure that the pandemic exerted on the healthcare system accelerated the search for creative solutions. Telemonitoring projects launched by hospitals and GP practices are a clear example. At the end of 2020 the Belgian National Institute for Health and Disability Insurance (NIHDI) rolled out the “telemonitoring convention for COVID-19 patients.” Participating organisations received a flat fee of €65 to €100 per monitored patient per week, depending on the care pathway and equipment.
The main objective was to relieve hospitals by avoiding or shortening admissions. Two pathways were defined. The prehospital pathway targeted patients presenting to their GP or the ED with COVID-19 symptoms who could recover at home provided that they were followed up remotely based on risk and symptom stratification. The posthospital pathway targeted patients discharged from hospital who still required structured home monitoring.
This pilot convention ended on 30 June 2022. The Belgian Health Care Knowledge Centre (KCE) evaluated the initiative and published an extensive report. Below we highlight the most relevant findings for primary care.
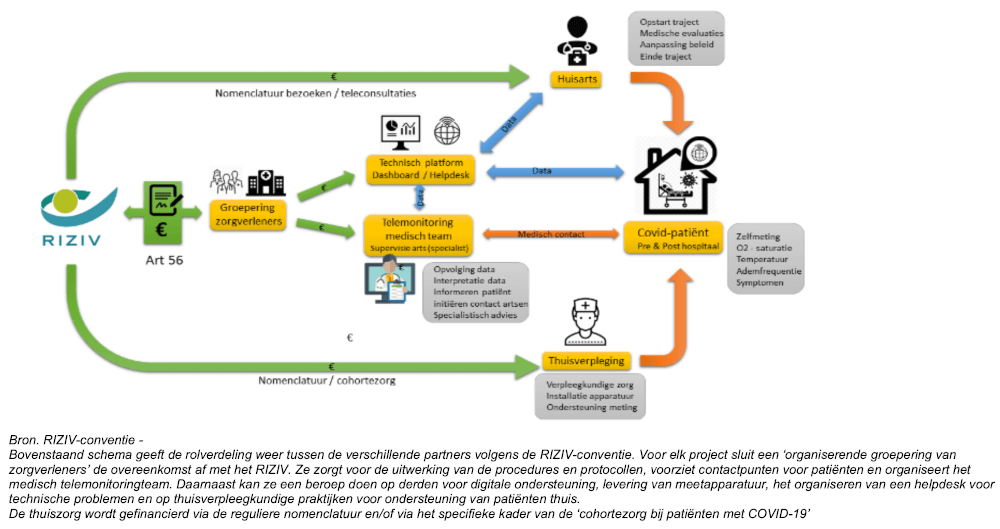
2. PROJECT SETUP
Twelve projects were analysed, eleven of which were coordinated by a hospital. The convention required close collaboration between first- and second-line caregivers: GPs, home nurses, the hospital, a telemonitoring unit, a technical team, and of course the patient. In practice, collaboration with first-line caregivers remained limited and telemonitoring teams only rarely contacted GPs directly.
Nevertheless, many GP practices launched their own telemonitoring initiatives without relying on the convention budget. SafeLink, the project that eventually monitored the largest patient group, is a well-known example.
3. WHAT DID TELEMONITORING LOOK LIKE?
Patients were followed remotely by a telemonitoring team embedded within one or multiple hospital departments or operated by an external organisation.
Telemetry typically consisted of monitoring oxygen saturation and body temperature combined with a daily questionnaire on symptoms such as dyspnoea or exercise intolerance. Parameters, questionnaires, frequency, and equipment differed per project, disease phase, and risk profile. Because COVID-19 was new, no validated stratification scales were available, forcing each team to define its own threshold values. Many teams struggled with false alerts and adjusted thresholds (for all patients or at individual level) to prevent alarm fatigue.
Communication between patient and monitoring team was organised in two ways. With passive communication patients received immediate feedback after entering their measurements via a colour code with instructions (orange = repeat after one hour, red = contact the GP, telemonitoring team, or ED). With active communication the team proactively reached out through SMS or phone calls, often multiple times per day.
4. PATIENT EXPERIENCE
Keep in mind that only a minority of COVID-19 patients were enrolled, so selection bias is possible.
Patients reported peace of mind and a sense of safety thanks to continuous follow-up. Personal contact and transparent communication with the monitoring team reinforced that feeling. They also expected their GP to remain involved, as GPs are seen as the caregivers with the most holistic view of the patient and custodians of the global medical record.
Using the devices and uploading data proved manageable for most patients. If technical issues occurred they could contact a home nurse or the monitoring team. Negative feedback mostly related to too many alerts or questionnaires that felt unnecessary.
5. HOW DID PRIMARY CARE EXPERIENCE IT?
All interviewed GPs valued telemonitoring and stressed the importance of involving them as much as possible. Their knowledge of the patient’s history and social context makes them a crucial link, certainly for high-risk patients. At the same time many GPs experienced a higher workload due to extra administration and workflow interruptions caused by alerts.
Home nurses were also positive about the concept and believe it will play a major role in the future. Sufficient capacity and a clear organisation of the nursing team are key. A major barrier for them was the lack of access to the telemonitoring dashboards and patient data.
6. OVERCOMING PATIENT RESISTANCE TO INNOVATION
Adopting new care pathways often triggers resistance. The KCE report lists several strategies to overcome innovation anxiety:
- Install and configure the app and devices together with the patient and practice how to perform measurements.
- Provide additional educational material such as a video or brochure.
- Offer an easily accessible helpdesk for technical support.
- Involve first-line caregivers with an existing therapeutic relationship in every phase of the monitoring pathway.
- Engage patients when designing and testing telemonitoring pathways to ensure usability.
7. LITERATURE AND FUTURE VISION BEYOND COVID-19
The report also reviewed international literature on the effectiveness and cost efficiency of telemonitoring for COVID-19. Many publications claim telemonitoring is cost-effective because it prevents or shortens admissions, but the lack of high-quality economic studies makes it impossible to calculate a robust cost-effectiveness ratio.
Therefore the KCE recommends creating a research framework for telemonitoring in general. That would allow policymakers to collect evidence on remote monitoring for COVID-19 and other pathologies (chronic, acute, preventive), standardise best practices, and identify which patient groups benefit from which building blocks. For example, it is still unclear what the incremental value of adding a pulse oximeter is on top of two SMS check-ins per day for achieving 30-day survival without hospitalisation.
8. CONCLUSION
The convention proved that remote monitoring of COVID-19 patients is feasible. Healthcare professionals are willing to expand telemonitoring to other pathologies and to build structural collaborations. Governments should support them by developing care pathways and investing in a long-term research framework.
Primary care has an essential role. GPs and home nurses are close to the patient and can improve adherence, yet they were often not sufficiently involved. Limited data sharing between first and second line is a major bottleneck; better integration is required to create efficient workflows.
The pandemic offered Belgian policymakers and many healthcare actors their first hands-on experience with telemonitoring. The question now is: will we build on that momentum?
9. REFERENCE
Cornelis J, Van Grootven B, Irusta LA, de Meester C, Christiaens W, Van Durme T, Dierckx de Casterlé B, van Achterberg T, Mistiaen P. Telemonitoring bij patiënten met COVID-19 – Synthese. Health Services Research (HSR). Brussels: Belgian Health Care Knowledge Centre (KCE). 2022. KCE Reports 354As. (KCE report)
Want to explore Co-Medic further?
Connect with our team or keep reading more insights from our blog archive.
Available in:
Related articles
Feb 5, 2026
Chronic kidney disease: from underdiagnosis to overview with population management
CKD is often insufficiently followed up in primary care. Population management helps identify and follow patients according to guidelines.
Read more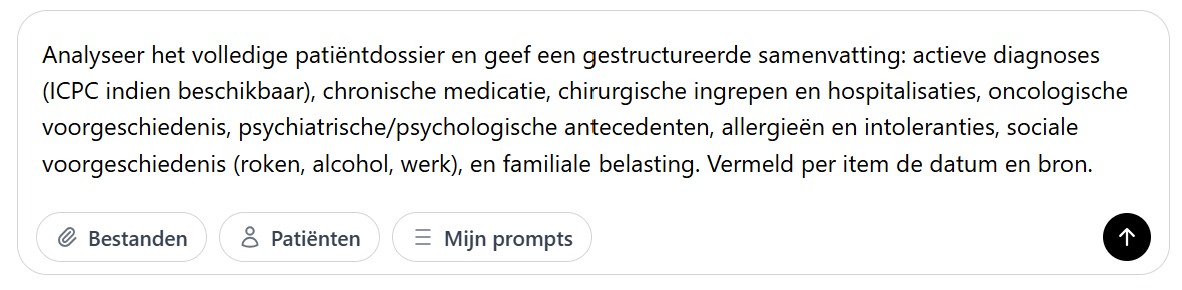
Jan 27, 2026
How Co-Chat relieves daily administrative tasks
Dr. Bram Spinnewijn shows how he writes referral letters during consultations with Co-Chat, without GDPR concerns.
Read more
Jan 20, 2026
Detecting (often hidden) heart failure in general practice with NLP
How natural language processing helps systematically identify heart failure, including the difficult-to-detect HFpEF variant, in electronic medical records.
Read more